AI-Powered Chatbot Enhances Member Portal for Health Plan
From long wait times to instant answers — how AI made member support faster, smarter, and compliant.
For regional health plans, delivering timely, accurate support to members is critical — especially
during peak enrollment periods when call centers are overwhelmed. A mid-sized Medicare Advantage plan
serving 20,000–30,000 members faced rising call volumes, frustrated seniors, and growing compliance
risks. To address these challenges, the plan partnered with Serious Development to deploy an AI-powered
chatbot inside its member portal. The solution delivered 24/7 self-service, simplified access to
CMS-required documents, and significantly reduced operational costs — while improving member
satisfaction and boosting Star Ratings.
PROJECT OVERVIEW
PROJECT DETAILS


Project Type
Custom Software Development
Technologies
AI/ML& NLP, Azure OpenAI APIs, CRM integrations, Azure Cloud
PROJECT SUMMARY
A mid-sized Medicare Advantage Prescription Drug (MAPD) health plan in the Western U.S.
struggled with high call center volumes, compliance risks, and member
frustration—particularly among seniors navigating complex CMS documents. Serious
Development implemented an AI-powered chatbot directly into the member portal, leveraging
Azure OpenAI APIs with retrieval-augmented generation (RAG). The chatbot provided 24/7
self-service in English and Spanish, securely integrated with the portal and CRM, and
ensured HIPAA and CMS compliance. Within six months, the health plan reduced inbound calls
by 25–30%, increased portal usage by 40%, resolved 70% of inquiries via chatbot, and
achieved annual savings of $300K–$480K, while improving member satisfaction.
“The chatbot didn’t just deflect calls — it transformed how we serve our members. Seniors can now
get clear, accurate answers any time of day, in their language, without waiting on hold. It’s
improved satisfaction, ensured compliance, and given our team room to focus on more complex care
needs.” — Chief Operating Officer, Regional MAPD Health Plan


THE CLIENT

Situational Overview
The client, a mid-sized Medicare Advantage Prescription Drug (MAPD) health plan in the Western
United States, served 20,000–30,000 members, primarily seniors. During peak enrollment periods,
the plan’s call centers were overwhelmed with routine inquiries about benefits, formularies,
and provider directories. Members faced long wait times, limited self-service outside business
hours, and difficulty navigating CMS-required documents. These challenges not only strained
operational resources and increased costs but also created compliance risks from inconsistent
responses. With CMS Star Ratings increasingly tied to member experience, the organization
needed a scalable solution to improve accessibility, reduce call volumes, and strengthen
compliance.

CHALLENGES
Overview
 CMS Compliance – Ensuring all chatbot responses were consistent, accurate, and sourced only from CMS-approved documents to avoid compliance risks.
CMS Compliance – Ensuring all chatbot responses were consistent, accurate, and sourced only from CMS-approved documents to avoid compliance risks.
 Senior Accessibility – Designing the chatbot with plain language, clear flows, and multilingual support (English + Spanish) to meet the needs of older members.
Senior Accessibility – Designing the chatbot with plain language, clear flows, and multilingual support (English + Spanish) to meet the needs of older members.
 Accuracy & Trust – Delivering reliable answers on benefits, formularies, and pharmacy questions using retrieval-augmented generation (RAG) and regular compliance reviews.
Accuracy & Trust – Delivering reliable answers on benefits, formularies, and pharmacy questions using retrieval-augmented generation (RAG) and regular compliance reviews.
DETAILS
There was a pressing need for a system that could handle increased demand and facilitate easier and faster service delivery.
THE SOLUTION
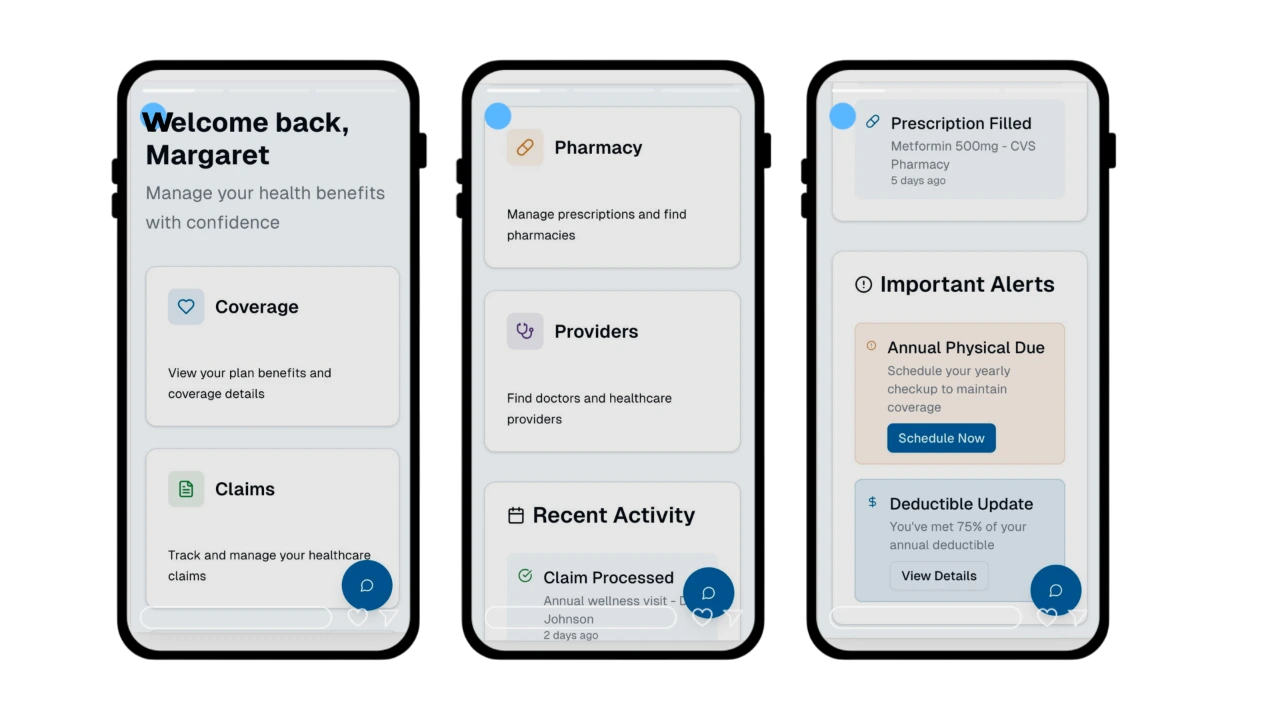
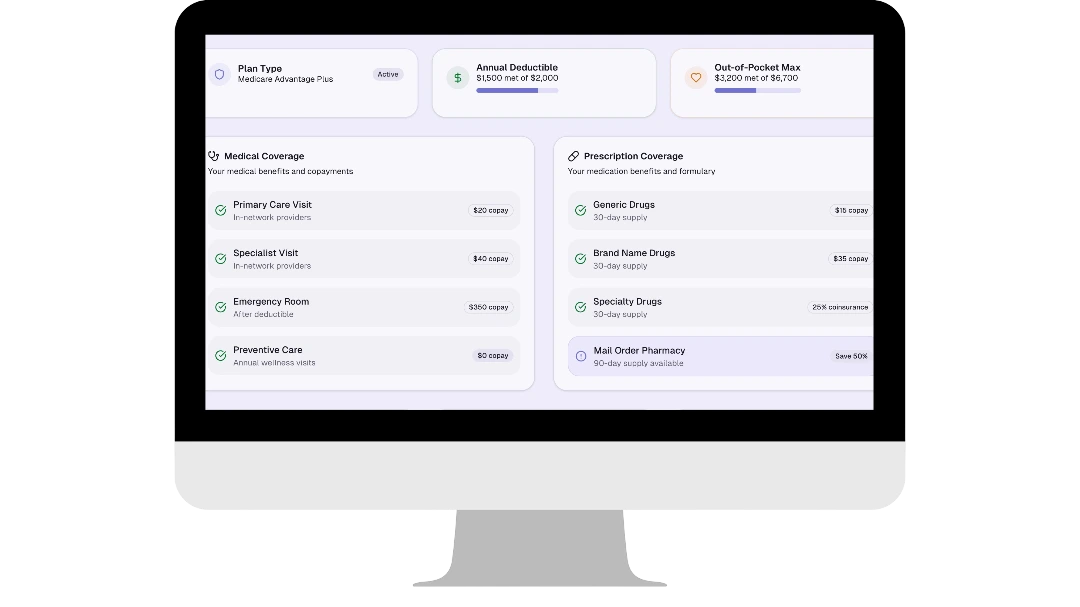 Serious Development designed and deployed an AI-powered chatbot within the member
portal to give seniors instant, accurate access to benefit and pharmacy information. Built on
Azure OpenAI APIs with retrieval-augmented generation (RAG), the chatbot delivered
conversational Q&A grounded in CMS-approved documents such as EOCs, formularies, and provider
directories.
Key features included:
Serious Development designed and deployed an AI-powered chatbot within the member
portal to give seniors instant, accurate access to benefit and pharmacy information. Built on
Azure OpenAI APIs with retrieval-augmented generation (RAG), the chatbot delivered
conversational Q&A grounded in CMS-approved documents such as EOCs, formularies, and provider
directories.
Key features included:
- Natural language processing for intuitive, human-like conversations.
- Bilingual support (English and Spanish) to improve accessibility.
- Escalation workflow for unresolved inquiries, with guaranteed response in 1–2 business days.
- Quarterly retraining based on call center trends and compliance reviews.
Results
A mid-sized Medicare Advantage Prescription Drug (MAPD) health plan serving 20,000–30,000 members partnered
with Serious Development to modernize its member portal. Seniors faced long call center wait times,
difficulty navigating CMS documents, and limited self-service options, which put compliance and Star
Ratings at risk. Serious Development delivered an AI-powered chatbot using Azure OpenAI APIs with
retrieval-augmented generation (RAG), integrated securely into the member portal and CRM.
Within six months of deployment, the chatbot:
- Reduced inbound calls/emails by 25–30%
- Resolved 70% of inquiries directly through the chatbot
- Increased portal usage by 40%
- Generated $300K–$480K in annual savings from call deflection
- Improved CMS Star Ratings by boosting member experience scores

“The chatbot didn’t just deflect calls — it transformed how we serve our members. Seniors can now get clear,
accurate answers any time of day, in their language, without waiting on hold. It’s improved satisfaction,
ensured compliance, and given our team room to focus on more complex care needs.” — Chief Operating Officer,
Regional MAPD Health Plan
 Quality
Quality
Contact Us
Please leave your contact information and we will get back to you as soon as possible.

Other Case Studies
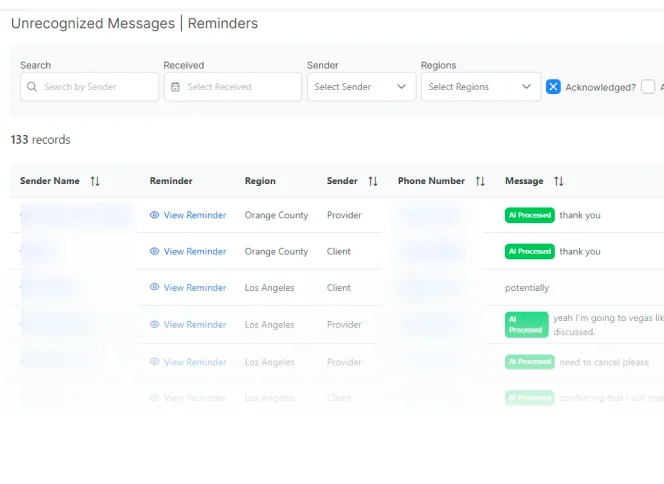
AI-Powered SMS and Email Messaging App
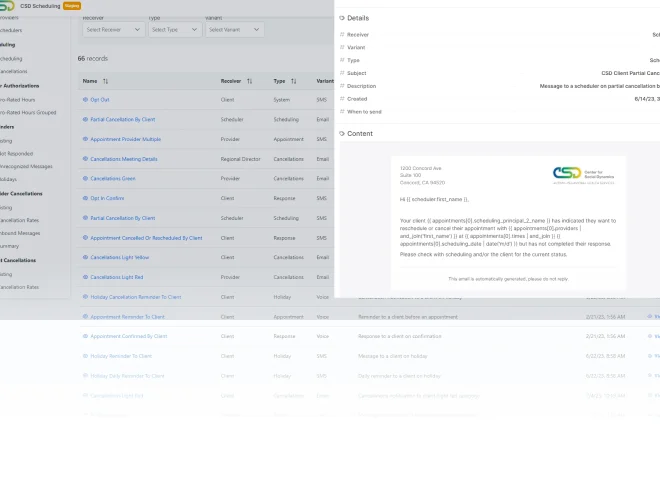
Client and Employee Scheduling App for ABA
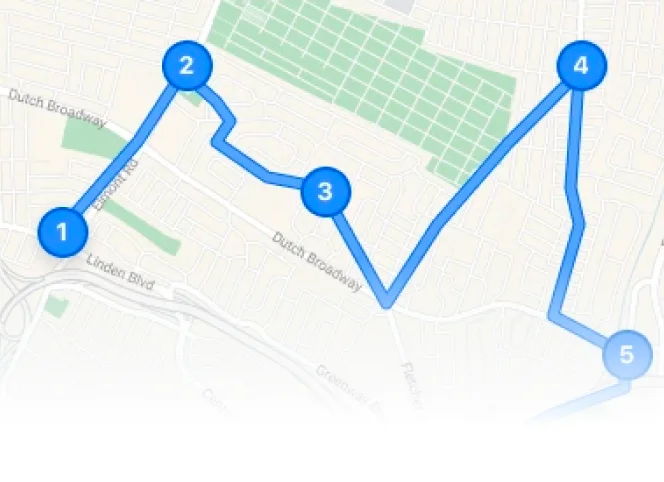
Scheduling and Map Routing App for Medical Clinic