Case Study: Automating Provider Onboarding Intake with AI: From 100-Page Packets to Credentialing-Ready Files
How a large MSO cut intake time by 75%, eliminated errors, and accelerated provider onboarding with a simple two-step AI pipeline.
For healthcare organizations, provider onboarding is both mission-critical and time-sensitive. Before a
provider can see patients, MSOs must validate their qualifications, licenses, and compliance with
regulatory standards. But the process starts long before credentialing — with the intake of onboarding
documents.
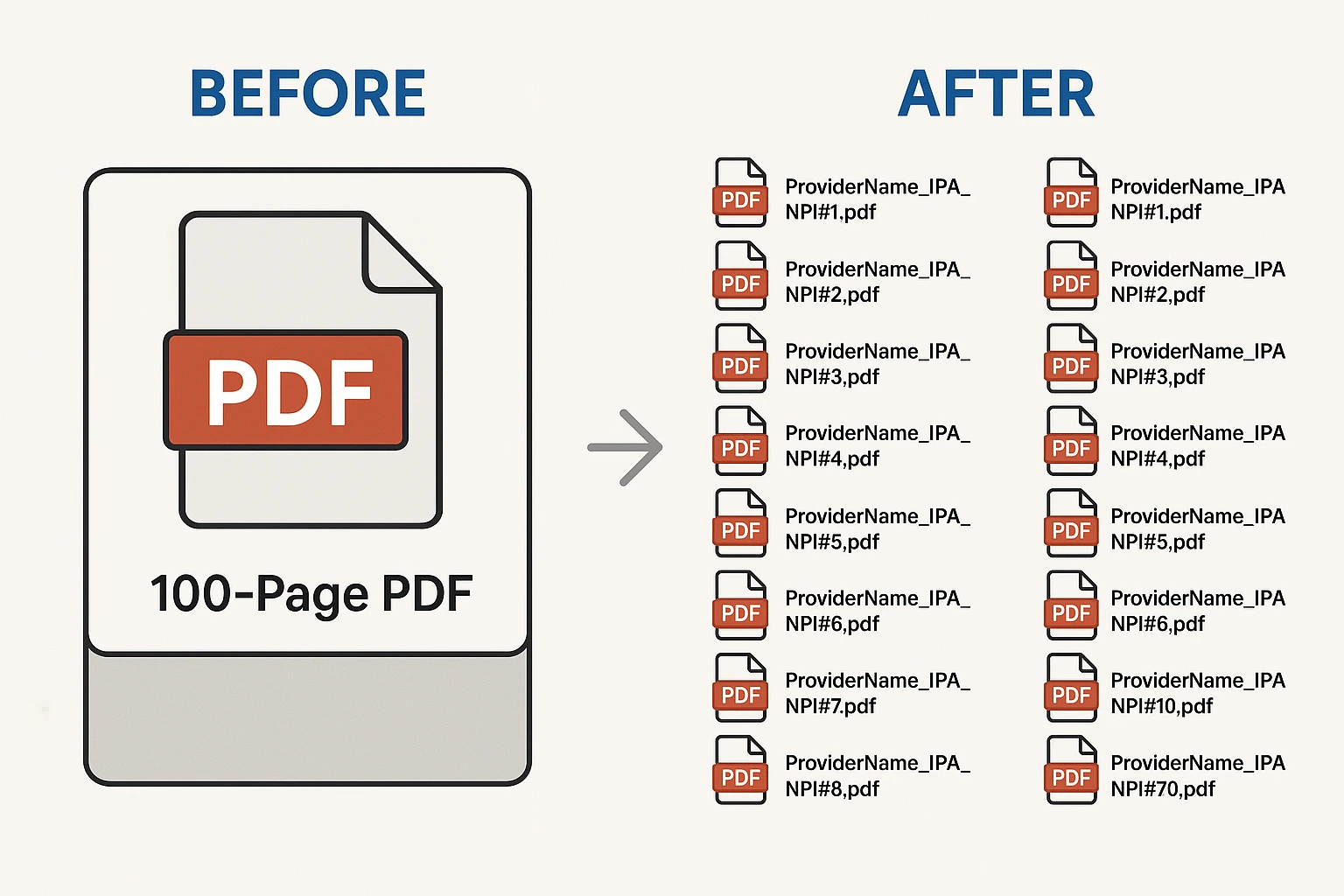
Our client, a large MSO, was drowning in unstructured onboarding packets ranging from 30 to 100+ pages. Each file was a mix of applications, state licenses, DEA certificates, diplomas, and insurance documents — all buried in a single PDF. Specialists had to manually scroll, split, rename, and file documents, a process that took up to 30 minutes per provider and introduced frequent errors.
The result: delayed onboarding timelines, compliance risks, and frustrated providers and staff. To break the bottleneck, the organization needed a smarter way to transform messy PDFs into clean, credentialing-ready files.
This case study shows how a lightweight, two-step AI pipeline delivered exactly that — cutting intake time by 75%, ensuring error-free files, and empowering staff to focus on higher-value work
Our client, a large MSO, was drowning in unstructured onboarding packets ranging from 30 to 100+ pages. Each file was a mix of applications, state licenses, DEA certificates, diplomas, and insurance documents — all buried in a single PDF. Specialists had to manually scroll, split, rename, and file documents, a process that took up to 30 minutes per provider and introduced frequent errors.
The result: delayed onboarding timelines, compliance risks, and frustrated providers and staff. To break the bottleneck, the organization needed a smarter way to transform messy PDFs into clean, credentialing-ready files.
This case study shows how a lightweight, two-step AI pipeline delivered exactly that — cutting intake time by 75%, ensuring error-free files, and empowering staff to focus on higher-value work
PROJECT OVERVIEW
PROJECT SUMMARY
A large MSO was struggling with the first step of provider onboarding: document intake.
Each new provider submitted a packet of 30–100+ pages containing applications, licenses,
DEA certificates, diplomas, and insurance documents — all in one unstructured PDF.
Specialists were forced to manually review, split, rename, and file documents, consuming
up to 30 minutes per provider and delaying credentialing timelines.
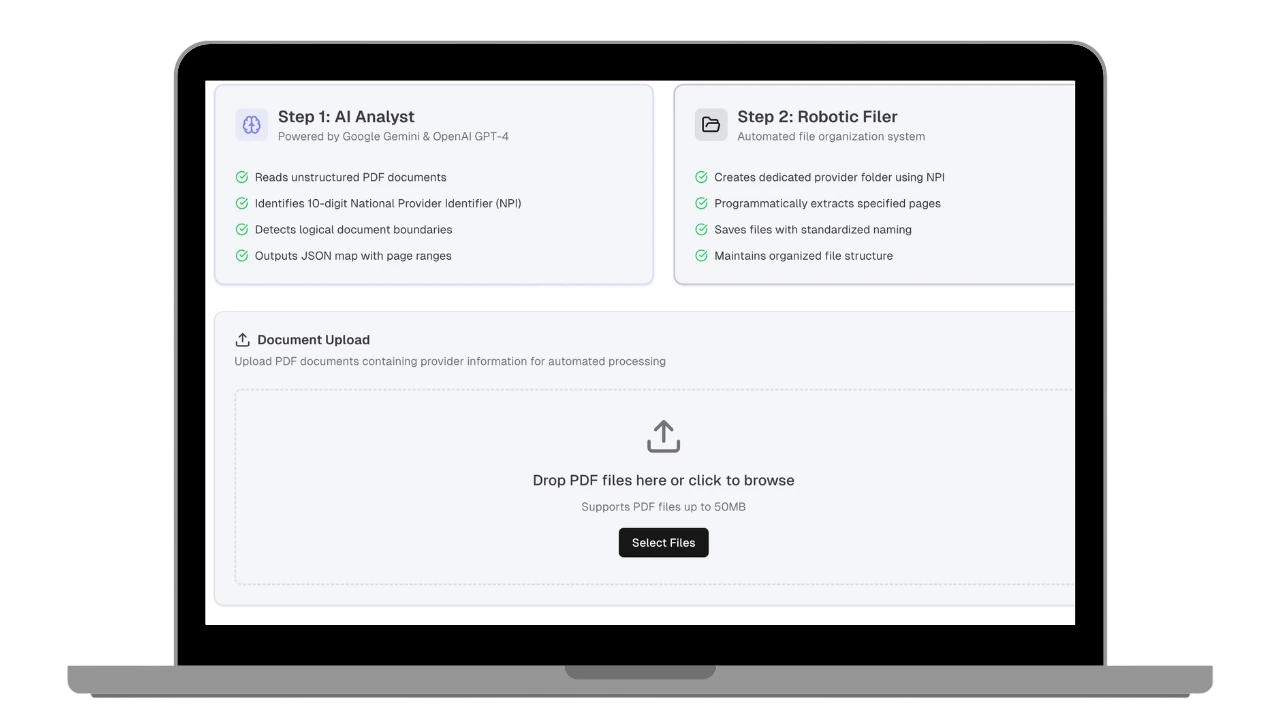
To solve this, we implemented a lightweight, two-step AI-powered pipeline.
A Python script with Large Language Models (GPT-4 and Gemini) acted as an “AI Analyst,”
detecting document boundaries, identifying the provider’s NPI, and outputting a JSON map
of files and page ranges. A second deterministic script — the “Robotic Filer” — executed
the plan by extracting pages, applying standardized naming, and filing documents
automatically.
The results were immediate: document intake was completed 75% faster, files were error-free
and compliant, scalability improved without additional staff, and specialists could focus
on higher-value validation. This project proved how targeted AI automation can turn one of
healthcare’s most frustrating administrative bottlenecks into a streamlined, reliable
workflow.


THE CLIENT

Situational Overview
Onboarding new providers is one of the most critical — and time-sensitive — administrative
processes in healthcare. Before a provider can see patients, MSOs must validate their
qualifications, licenses, and compliance with regulatory standards. But the first step is
document intake: transforming unstructured provider packets into a clean, credentialing-ready
file set.
This MSO was inundated with onboarding packets that were 30 to 100+ pages long. Each contained
a mix of application forms, state licenses, DEA certificates, diplomas, and liability insurance
documents — all buried in a single file.
Specialists were forced to manually scroll through each packet, split documents page by page,
rename files according to strict conventions, and store them in the correct folders. This
manual approach:
- Consumed up to 30 minutes per provider.
- Delayed onboarding and credentialing timelines.
- Introduced human error.
- Left staff frustrated with repetitive administrative work.

CHALLENGES
Overview



Time-Consuming Manual Intake
Onboarding specialists spent 20–30 minutes per packet scrolling, splitting, renaming,
and filing documents. With dozens of providers onboarded each month, this created
significant delays.
Downstream Errors for Credentialing
Manual intake often led to misplaced or mislabeled files, which then slowed down
credentialing teams and introduced compliance risks.
Scalability & Staff Morale
Skilled employees were bogged down by repetitive administrative tasks. Scaling
onboarding volume would have required hiring more staff, increasing costs and lowering
morale.
THE SOLUTION
 We designed a lightweight, two-step AI-powered pipeline that streamlined provider onboarding intake
without requiring a large-scale system overhaul.
We designed a lightweight, two-step AI-powered pipeline that streamlined provider onboarding intake
without requiring a large-scale system overhaul.
- A Python script leveraged Large Language Models (GPT-4 and Gemini) to read entire unstructured PDFs and generate structured instructions.
- Identified the provider’s National Provider Identifier (NPI).
- Detected logical document boundaries (application, license, DEA certificate, insurance).
- Output a JSON “map” of document names and page ranges.
- A second deterministic script executed the AI’s instructions with complete accuracy.
- Created a dedicated provider folder using the NPI.
- Programmatically extracted and split documents.
- Saved each file under standardized naming conventions.
Results
This modular approach balanced the power of AI with the reliability of rule-based automation, ensuring both
speed and precision.
- 75% faster document intake → Providers moved into credentialing more quickly.
- Error-free file preparation → Credentialing teams got clean, compliant data.
- No extra headcount needed → Scalability achieved without adding staff.
- Happier specialists → Employees were freed from repetitive admin tasks and could focus on higher-value validation.
- Happier Providers → Seeing new patients faster.
SUMMARY
By automating the intake of complex provider packets, this MSO turned one of its biggest onboarding
bottlenecks into a streamlined, scalable process. The two-step AI pipeline reduced intake time by 75%,
ensured error-free, credentialing-ready files, and allowed credentialing teams to work faster with greater
confidence.
The impact went beyond efficiency: specialists no longer wasted time on repetitive administrative tasks,
onboarding timelines shortened across the board, and the organization avoided adding headcount while
scaling provider volume.
This case study demonstrates how targeted AI automation — even applied to something as basic as PDF
intake — can deliver measurable results in speed, compliance, and staff satisfaction. For healthcare
organizations under pressure to do more with less, it’s proof that the right blend of AI and automation
can make critical processes both faster and smarter.

“The automation completely changed how we handle provider onboarding. What used to take 20–30 minutes per
packet now happens in just a few minutes. Our credentialing team starts with cleaner data, and our
onboarding timelines are shorter across the board. This is a true win for efficiency, compliance, and staff
morale.”
 Quality
Quality
Contact Us
Please leave your contact information and we will get back to you as soon as possible.

Other Case Studies
AI-Powered SMS and Email Messaging App
Client and Employee Scheduling App for ABA
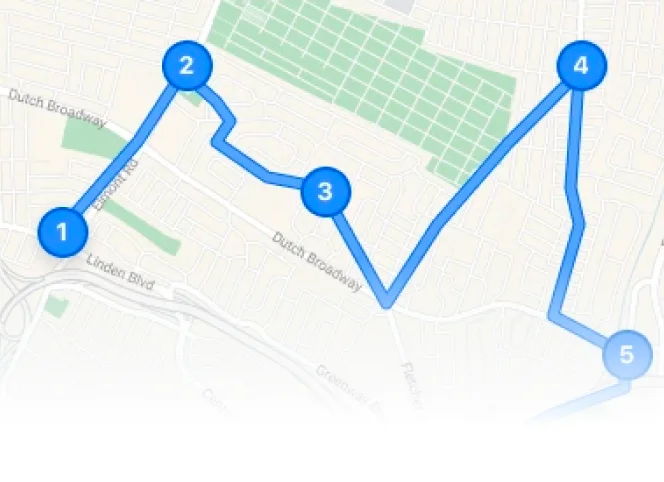
Scheduling and Map Routing App for Medical Clinic